
A new era in the management of osteoarthritis
Osteoarthritis (OA) is the most prevalent joint disease. It causes pain and disability in a large proportion of the population worldwide. It is considered as the most consequential rheumatic condition in terms of social -economic impacts. The incidence of the disease increases with age. The disease evolves over decades to end by the loss of joint function. In addition, aging patients present various co-morbid conditions that add to the complexity of the treatment of OA patients.
To date, there is no cure for OA. The only available treatments aim at reducing symptoms, as pain and inflammation, maintain joint mobility and limit the loss of function. The main goals that the ideal OA treatment has to achieve are symptom-modifying effect, reducing pain and inflammation, and structure-modifying effect, sparing joint structure and preventing joint degradation in order to maintain articular function.
Several guidelines, as the European League Against Rheumatism (EULAR), the American College of Rheumatology (ACR) or the Osteoarthritis Research Society International (OARSI) recommendations for the management of knee OA have been published for OA management. They all recommend both non-pharmacological and pharmacological approaches. The non-pharmacological interventions include education and self-management, regular telephone contact, referral to a physical therapist, aerobic, muscle strengthening and water-based exercises, weight reduction, walking aids, knee braces, footwear and insoles, thermal modalities, transcutaneous electrical nerve stimulation and acupuncture. The pharmacological treatments consist of acetaminophen, cyclooxygenase-2 (COX-2) non-selective and selective oral non-steroidal anti-inflammatory drugs (NSAIDs), topical NSAIDs and capsaicin, intra-articular injections of corticosteroids and hyaluronates, glucosamine and/or chondroitin sulphate, and avocado/soybean unsaponifiables (ASU) for symptom relief; glucosamine sulphate, chondroitin sulphate and diacerein for possible structure-modifying effects and the use of opioid analgesics for the treatment of refractory pain. Most of the pharmacological treatments available to relieve OA symptoms present serious adverse events, as the risk of gastro-intestinal or cardiovascular adverse events with NSAIDs. Moreover, this disease implies treatment or drug intake for decades, increasing the risk of serious adverse events and the incidence of co-morbidity factors.
Many efforts have been developed to find a cure to OA that can satisfy all the above-mentioned goals. The perfect drug would be not only able to relieve inflammation and pain but also to slow down, stop or even better prevent disease progression. This would result in the maintenance of joint function, sparing joint structures involved in OA, meaning cartilage, synovial membrane and subchondral bone.
Indeed, there is a strong necessity for prevention of OA. The first step passes by healthy lifestyle, weight loss and nutrition, with specific nutrients that could help to achieve this goal. Nutraceuticals are good candidates to help patient preventing OA or managing their disease using them as treatment adjuvant. Nutraceutical comes from the combination of the words nutrition and pharmaceutical. It corresponds to food or food product that provide health and medical benefits, including prevention and treatment6,7. By definition and regulatory laws they are devoid of adverse effects.
Nutraceuticals are good candidates for long-term prevention of chronic disease, such as OA. It is more and more recognized that nutraceuticals could help to maintain bone and joint health.
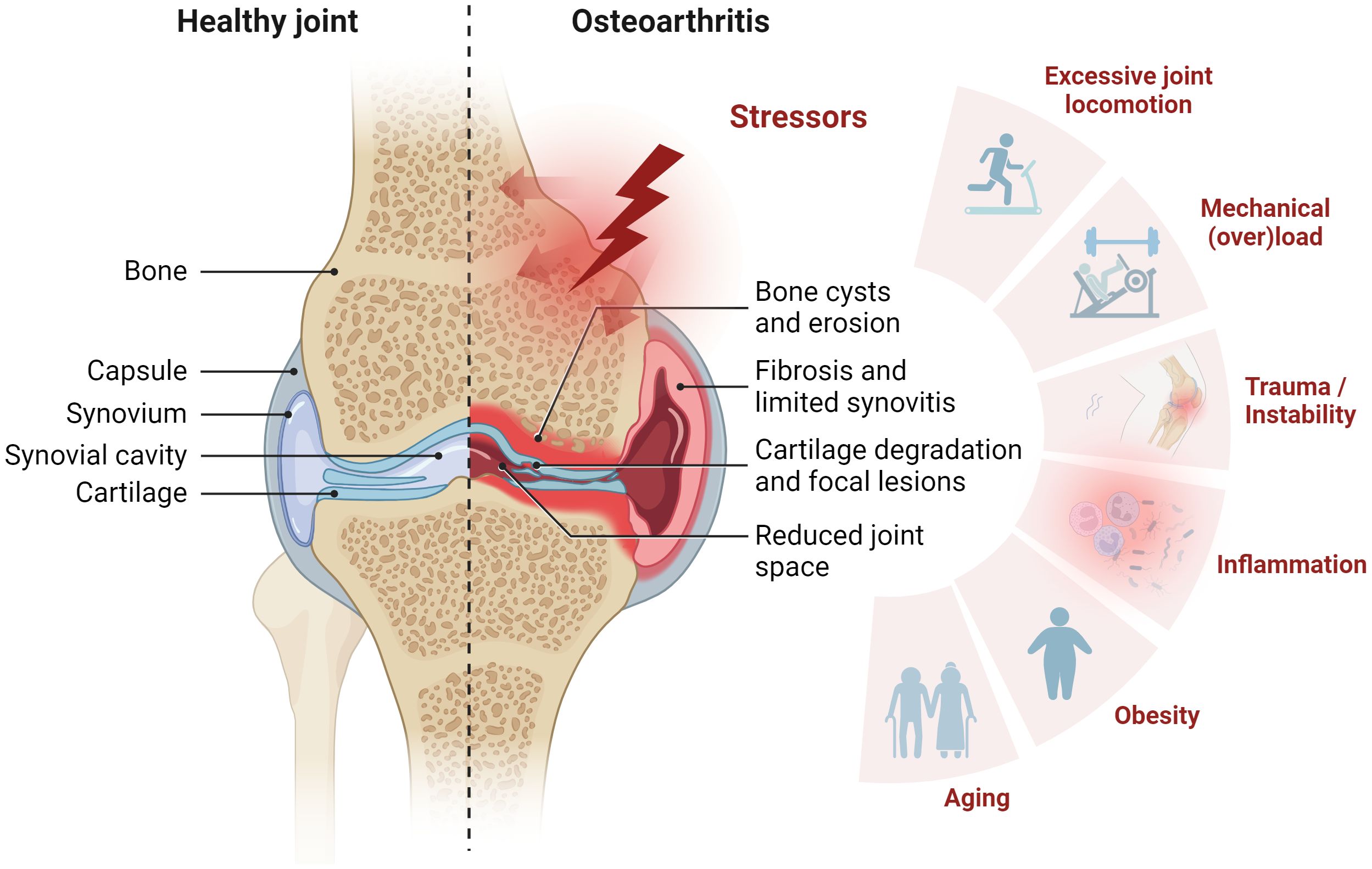
Articular structures of a synovial joint (knee joint example). Healthy tissues (left) and changes to joint tissues in OA (right). In a healthy joint, cartilage maintains its structural integrity. The subchondral bone turnover is tightly regulated, and the joint cavity has no signs of synovial inflammation. In contrast, the OA-affected joint exhibits pathogenic changes, which may include the presence of subchondral bone cysts, degeneration and thinning of cartilage, altered chondrocyte activity, synovial inflammation, and dysregulated bone turnover that may promote bone spurs. These alterations collectively contribute to the pathogenesis of OA and highlight the multifaceted nature of joint tissue changes in this condition.
CH is obtained by the enzymatic hydrolysis of collagenous tissues (bone, hide or hide split) form mammals. The main characteristic of CH is its amino acid composition, which is identical to type II collagen, thus providing high levels of glycine and proline, two amino acids essential for the stability and regeneration of cartilage. This product is generally recognized as a safe food ingredient by regulatory agencies. CH is well digested and is preferentially accumulated in cartilage. Although clinical use of CH is associated with minimal adverse effects, some gastro-intestinal side effects, as fullness and unpleasant taste, have been described. Clinical data Only three relevant CTs were identified in the literature. The first study investigated the effect of CH supplementation in healthy adult without degenerative joint disease but with joint pain. This study showed that CH dietary supplement can improve joint pain, mobility and reduce analgesic medication in healthy active adults without degenerative joint disease. The CH supplementation can then improve knee function during joint-stressing activities. The second report of medium methodological quality (score: 9)mentioned a better effect of CH compared to placebo in severe OA patients than in the overall studied population. More recently, in another relevant CT of very good methodological quality (score: 13), the joint function improvement after CH treatment was shown in patients with primary OA.
Vitamin DOA was traditionally considered as a cartilage disease, characterized by cartilage degeneration. But many evidences, as osteophytosis, subchondral bone sclerosis and cyst formation have grown up and demonstrated the prominent role played by subchondral bone in OA pathophysiology. Normal bone metabolism depends on the presence of vitamin D, a compound derived mostly from cutaneous exposure to ultraviolet and from the diet in a lesser extent. Suboptimal levels of vitamin D may have adverse effects on calcium metabolism, osteoblastic activity, matrix ossification and bone density. Low serum levels of vitamin D may increase the progression of knee OA and may impair the ability of bone to respond optimally to OA pathophysiologic processes and may predispose patients to joint degradation. High prevalence of low vitamin D status has been demonstrated in persons with knee OA. Moreover, in low bone mineral density (BMD) patient, the level of vitamin D seemed to influence the incidence and progression of the disease.
Devil’s Claw (Harpagophytum procumbens)Harpagophytum procumbens is a highly valued medicinal plant in southern Africa as well as the entire world. The body of evidence has shown that Devil’s claw plants are richly endowed with anti-cholesterolemic, antioxidant, anti-inflammatory, and pain killing effects for the therapeutic treatment of countless diseases including rheumatoid arthritis, memory loss, lower back pain, osteoarthritis, lumbago, Syphilis, diabetes, indigestion, and heartburn, as well as acting as a detoxifying and tonic agent. Toxicological data have shown that H. procumbens has adverse effects in high concentrations and various models promote low dose levels as a safety parameter.
Rosehip extractRosehip powder is an effective nutraceutical for treatment of OA patients because of its anti-inflammatory, chondroprotective and immune-modulatory action.
The role of Boswellia in various health conditions like inflammatory diseases, cancers, wound healing and antimicrobial activity is well known. The gum resin is extracted from the ancient herb, Boswellia serrata. It has been found to be a potent antiinflammatory, anti-arthritic and analgesic agent.
Summary points- ⦁ Calcium and vitamin D supplementation leads to a modest reduction in fractures, but use of calcium supplementation alone is not robustly supported.
- ⦁ The evidence for calcium and vitamin D supplementation for fracture reduction is most robust in those who are likely to be at greatest risk of calcium and/ or vitamin D insufficiency.
- ⦁ Although calcium is intimately involved in muscle physiology, the best clinical evidence suggests that vitamin D optimisation, rather than supplementation with calcium, leads to reduced risk of falls.
- ⦁ Calcium supplements are associated with gastrointestinal side-effects, and a small increased risk of renal stones.
- ⦁ The assertion that calcium with vitamin D supplementation increases cardiovascular risk is based on inadequate evidence; several studies demonstrate the converse or no cardiovascular effect.
- ⦁ Daily oral supplementation 800 IU of vitamin D3 plus 1200 mg of calcium reduces hip fracture and non-vertebral fracture in older people.
